Your Complete Guide to Vaginal Health: Understand, Care, and Flourish with Confidence
Discover tips, probiotics & care routines for better vaginal health. RadiumCare helps you feel confident, balanced, and infection-free every day.
2/5/20268 min read


Vaginal health is among the most important parts of a woman’s overall wellness, yet it’s usually not mentioned or talked about in a low voice. So many women are shy to discuss vaginal pain, discharge, infection, or discomfort—either because of stigma or insufficient information. But knowing how your body works is the key to improved health and self-confidence.
All women, by age or activity, will have changes in her vaginal health due to stress, hygiene, sexual activity, or self-evident hormones. Research indicates that approximately 75% of women will encounter some type of vaginal infection at some point during their lives. The good news is that most are preventable and treatable with proper care, habits, and knowledge.
At RadiumCare, we aim to shatter the stigma and help women obtain control back over their intimate wellness. With this complete guide, you are going to learn everything about the types of discharge, infections, hygiene, normal pH, and when to see your gynecologist.
What Is Vaginal Health and Why Does It Matter?
Vaginal well-being is the process of keeping the vagina, and the area around it, clean, well-balanced, and infection-free. The vagina cleanses itself and is lined with healthy bacteria (predominantly lactobacilli) that maintain the pH in slightly acidic (3.8-4.5) form. This acidity protects by preventing excessive growth of bad bacteria.
Disturbances in this equilibrium can bring about irritation, discomfort, or infections. They could be brought about by antibiotics, unsafe sex, hormonal changes, or bad hygiene practices. That’s why vaginal care is not all about cleanliness—it’s about guarding your immunity, reproductive health, and mental well-being as well.
What Is Normal Vaginal Discharge?
Discharge the body is the body’s way of naturally cleaning out your reproductive system, including scraping dead cells and bacteria, which helps keep the vagina healthy. Normal discharge will be different depending on where you are in your menstrual cycle, or may differ in terms of color, consistency, or the amount of discharge you may be experiencing.
Typical clear or milky white discharge should be colorless, and it typically has no odor. The stringy, stretchy, egg-white colored texture of discharge may also be experienced during your ovulation phase. Discharge may also become creamy or thicker right before your period. Discharge can also take on a yellow, green, or gray color, but if you notice a strong odor then this can be a sign of an infection and requires treatment.
Additionally, a white, cottage cheese-like discharge often indicates a yeast infection. Brown spotting may appear before or after periods—this is usually harmless unless it occurs frequently or with other symptoms like pain or odor.
Discharge is your vagina’s natural way of cleansing itself. It may vary throughout your cycle but usually falls within these ranges:
💡Tip: Discharge that has no smell or discomfort is usually probably not a problem. If your discharge changes in smell, color, or consistency–or causes itching, burning, or pain–please talk to a healthcare professional.
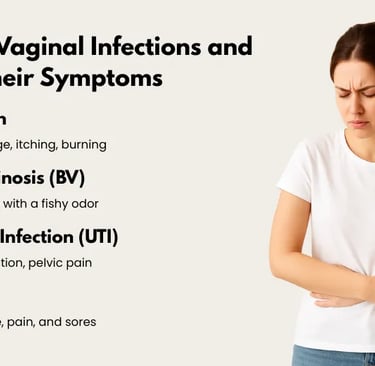
Common Vaginal Infections and Their Symptoms
The majority of women at some time in life suffer from vaginal infection. The most prevalent include yeast infection, bacterial vaginosis (BV), urinary tract infection (UTI), and sexually transmitted infection (STI).
Yeast infection results from Candida albicans overgrowth, a fungus. Symptoms are thick, white discharge, itching, burning, and pain. It may be treated with vaginal tablets or antifungal creams.
Bacterial vaginosis (BV) arises when there is an overproduction of the usual bacteria found in the vagina. Thin, grayish discharge with a fishy smell, most noticeable after sex, characterizes it. Antibiotics like clindamycin or metronidazole are often used to treat BV.
Not a vaginal infection per se, a UTI will frequently result in burning on urination, frequent urination, and pain in the pelvis. Bacteria that enter the urinary tract cause UTIs, and such entry is often the result of poor personal hygiene or post-coital exposure.
A few STIs, including chlamydia, gonorrhea, or trichomoniasis, may also result in abnormal discharge, pain, and sores. These need to be tested immediately and treated appropriately

The Role of Vaginal pH in Preventing Infections
Your vaginal pH is a reliable indicator of vaginal health! Healthy vaginal pH (3.8–4.5) maintains the prevalence of favorable bacteria while inhibiting the proliferation of pathogenic microorganisms. Life events, however, as well as some of your daily routines, influence this equilibrium.
Unprotected sex (semen is alkaline), repeated antibiotic use, douching, or use of synthetic underwear may cause pH disturbance. Menstruation and menopause both affect vaginal conditions as a result of endocrine fluctuations.
When your pH is out of balance, you can get itching, burning, odor, or infection. Your gynecologist may then prescribe pH-balancing vaginal suppositories or antibiotic creams. Use them only as directed and never use over-the-counter products without a doctor’s advice.
Proper Vaginal Hygiene: Simple Dos and Don’ts
Proper hygiene is crucial to keep the vaginal area healthy. Many women unknowingly damage their intimate part by using strong soaps, scented products, or douching.
Always wash just the outside vulva only—never within the vaginal canal. Lukewarm water and, if necessary, a fragrance-free mild cleanser are fine. Do not use scented wipes, powders, or sprays because these products can irritate the thin skin and throw off pH.
Wear airy cotton underwear and do not wear tight clothing for extended periods of time. Immediately change out of wet clothing or sweat-stained gym attire. Rinse underwear completely to prevent leaving behind detergent residue.
After exercise or sexual activity, clean gently and void immediately afterwards to reduce the risk of UTIs. Avoid using hair removal cream on the vaginal area frequently, as this may lead to burning or drying.
Menstrual Care and Its Effect on Vaginal Health
Your menstrual cycle is very closely related to vaginal health. Hormonal fluctuations during menstruation can cause heightened sensitivity, changes in discharge, or dryness. Proper maintenance of personal hygiene during menstruation is essential to prevent irritation and infection.
Always use unscented pads or tampons, and replace them at every 4–6 hours even if the menstruation is light. Never re-use the same sanitary pad or tampon for the entire night because it may be infested with bacteria and cause rashes or infection.
Do not use fragrant sanitary napkins, tampons, or menstrual cups. They can disrupt the vaginal flora. Keep it dry and clean and wash your hands before and after handling menstrual products.
How Hormones Affect Vaginal Wellness
Estrogen and the other female hormones are what keep your vagina healthy, elastic, and lubricated. Hormones move at different phases in life—puberty, pregnancy, lactation, and menopause—and will have an impact on vaginal tissues.
For example, reduced levels of estrogen during menopause can lead to dryness, vaginal thinning, and painful sex. Breastfeeding women might even suffer from temporary dryness because of decreased estrogen.
To maintain hormonal health, follow a balanced diet that contains phytoestrogens (such as soybeans, sesame, flaxseeds), remain physically active, and reduce stress. In certain situations, estrogen creams or vaginal moisturizers may be prescribed by your doctor.
The Mind-Body Connection: Stress and Vaginal Health
Stress is not only a psychological condition—it’s a bodywide phenomenon, including your sex life. Chronic stress lowers your immunity, disrupts your hormonal balance, and increases your susceptibility to infections.
Stress can also present with physical manifestations like vaginal dryness, low libido, irregular menstrual cycles, or pelvic pain. To help manage anxiety, try to include relaxation activities in your daily schedule whenever you can. Examples of relaxation activities include yoga, deep breathing, journaling or meditation.
Emotional well-being is a vital aspect of overall gynecologic well-being. If you are suffering from anxiety disorders or body image dysfunctions, you might also want to investigate a consultation with a psychotherapist, counselor or therapist for further assistance, especially if these could impact your affect towards having sexual relations.
When Should You Visit a Gynecologist?
Some vaginal concerns can be self-treated, but others have to be attended to by experts. Do not self-medicate the recurring symptoms or the body changes that will not disappear with simple remedies.
Visit a gynecologist if you experience:
Recurring burning, itching, or dryness
Colored or foul-smelling discharge
Painful urination or sex
Spontaneous bleeding or spotting
Recurring swelling, lumps, or sores in the vagina
Recurring infection despite good hygiene
Your doctor can use tools such as a vaginal speculum to examine your cervical walls and vaginal walls during a gynecology appointment. Although it may sound frightening, it is painless and only takes a minute or two.
Quick Daily Checklist for Vaginal Health
Following is a patient educational checklist that keeps you in charge of your intimate health:
Use soap and water to wash vagina or mild soap
Use cotton underwear and change them daily
Avoid scented products, douching, or strong chemicals
Remember to stay on a healthy, balanced diet with lots of water.
Track your menstrual cycle and report any changes
Treat irregular discharge, pain, or odor.
Apply vaginal creams, pessaries, or tablets only on the advice of your doctor
Have safe sex and adopt open communication with your partner.
Deal with stress and take care of mental health
Ensure to visit a gynecologist for preventive visits at least once annually
Final Thoughts: Embrace Your Health, Embrace Yourself
There is no shame in your vagina—it’s a strong, intelligent, and integral part of your body that deserves to be treated with careful consideration, responsible attention, and worthy respect. Vaginal health, or discomfort prevention, is not something to ‘get it done’; it’s an unflinching embracement of an integral part of who you are, and your well-being.Your vagina is communicating with you at all times, from hormonal responses to normal discharge. Being able to recognize those messages creates a sense of security, comfort, and empowerment. Let’s deconstruct the shame and acknowledge that vaginal wellness is a vital aspect of one’s well-being that deserves the same notice we take of other dimensions of well-being – openly and shamelessly.
One lesser-known but powerful way to preserve intimate wellness is through the use of Lactobacillus-filled vaginal tablets. These healthy probiotics keep the vaginal microbiome healthy by:
Restoring and rebalancing vaginal pH
Replacing defensive good bacteria to assist in protecting against infection
Preventing recurrent symptoms such as bacterial vaginosis and yeast infections
Aiding healing after antibiotic courses or hormonal changes
Boosting natural defense systems for long-term comfort and confidence
Whether you’re identifying infection signs, balancing dryness, or interpreting changes in your discharge, trusting your body allows you to take proactive steps rather than responding too late. Discomfort is never something you need to “just live with.” With the proper information, timely treatment, and guidance of effective solutions such as probiotics, it’s possible to balance, prevent recurrences, and achieve intimate health throughout each stage of life.
At RadiumCare, we believe in the idea that every woman does not only deserve to be treated, but also heard, educated, and trusted by her own body. We aim to make the conversation of vaginal health the norm and a powerful part of daily wellness. Whether you’re going through hormonal changes, postpartum adjustments, or just maintaining personal hygiene on a daily basis, you are not alone. Your journey of health is legitimate, deserving, and wholeheartedly something to be celebrated.
Let’s love our bodies, take care of our well-being, and move from silence to strength—because intimate health is self-care, and self-care is a powerful thing.
Disclaimer:
This article is for general information only and must not be used as a replacement for guidance from a qualified medical practitioner. Always consult your gynecologist prior to using vaginal creams, tablets, pessaries, or home remedies.
Frequently asked questions
What are the indicators of an unhealthy vaginal microbiome?
Common symptoms include abnormal discharge, odor, itching, burning, swelling, and recurrent infection such as BV or yeast infection. Some of them also have pain during sex or during urination.
How do vaginal probiotics such as Lactobacillus benefit?
They keep the pH healthy, inhibit pathogenic bacteria from dominating, and defend against the immune system—preventing BV, yeast infection, and vaginal health.
Can I take vaginal probiotics on my period?
Yes, you can. They’re generally safe, though some will discontinue use of suppositories. Regular use maintains vaginal balance even while you’re in your cycle.
How can I maintain good vaginal hygiene daily?
Use mild cleansers, do not douche, and use cotton undergarments. Probiotics may also be used to maintain healthy vaginal flora and balance.
Phone no. +91-84343 84343
Support: [email protected]
Location: 40-GF, Harmony Mall, Goregaon (W), Mumbai – 400


A Gentle Touch for Motherhood
Pregnancy-safe, thoughtfully crafted skin and personal care solutions designed to support women through every stage of motherhood.
Quick Links
Get in Touch
