How to Read a Medication Label: A Complete Guide for Safer Use
Learn how to read medication labels properly — know drug names, dosage, expiry, routes & warnings. Stay safer with Radium Care’s complete guide.
2/5/20269 min read


Each of the medications you find in a hospital, clinic, or drug store has a label attached to it. It is not only a sticker — it is a safety guide that includes all the information you need about the medication: what it is, how to take it, who can take it, and when not to use it.
For doctors, nurses, pharmacists and caregivers, reading and understanding a label on a medication is an important first step to ensure safe treatment. Even to patients, learning this can help avoid errors and boost confidence. Misreading or neglecting a single detail could result in incorrect dosages, improper administration, or even life-threatening scenarios.
A drug label contains important information like the trade name and generic name, strength of the dose, form of the drug, and route of administration. It also states instructions for how to safely administer it, how to store it under the right conditions, and the expiration date, to help it work correctly. There are labels that contain warnings about safety, batch numbers to track batches, and identification codes to avoid counterfeit drugs.
In medicine, a single small error in reading or interpreting a label can lead to severe risks. For instance, confusing two drugs that have similar names, forgetting the strength of the dosage, or forgetting whether the drug needs to be consumed with food or on an empty stomach can all cause treatment failures or side effects.
At Radium Care, we believe that education around this subject is the first step to safer healthcare. Patients will go from being solely reliant on the care they receive to a point of taking responsibility for their own health through training to read and understand medication labels. Healthcare staff will be able to provide safer and better care. Let’s take it one step at a time, and break down the most important parts of a medication label.
What is a Medication Label?
A label on a medication is the officially printed text on a pack, strip, vial, or bottle of medicine. It guarantees that:
The correct drug finds the correct patient.
Dosage and administration are correct.
Medicines are kept under safe conditions.
Expired or recalled batches are avoided.
Reading the label is not merely compliance, but it is about safeguarding health and saving lives.
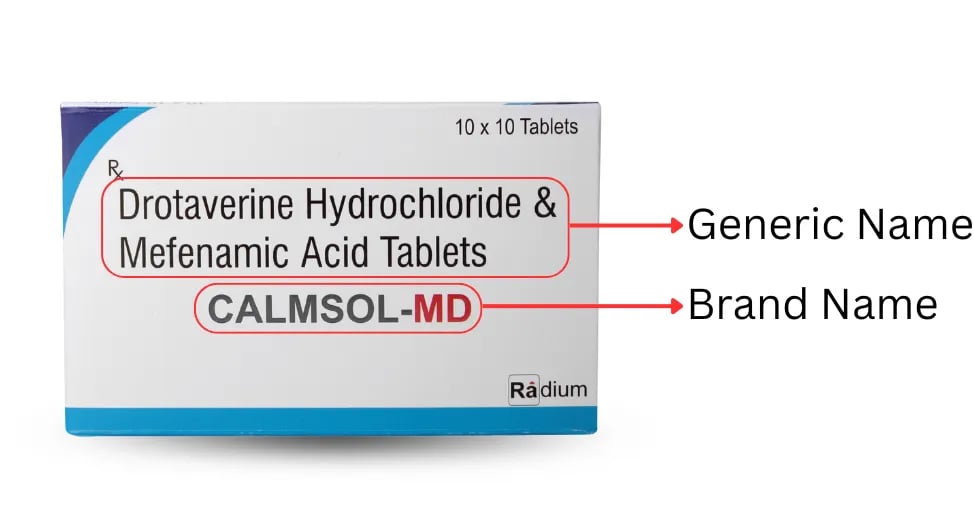
1. Brand Name vs. Generic Name
Brand Name (or Trade Name):
It is the name under which the drug is registered by the company. It is patent protected, meaning no generic drug can be produced until the patent is over. Brand names are often short, simple to pronounce, and in bold or uppercase letters.
Example: Calmsol-MD
Generic Name:
This is the active constituent of the drug. Generic names are longer, more difficult to pronounce, and in smaller or lower case letters. There is a single generic name for each drug, but it can be marketed under various brand names.
Example: Mefenamic Acid 250 mg + Drotaverine Hydrochloride 80 mg (the generic name in Calmsol).
Why it is important: Patients need to be aware that generic drugs tend to be less expensive but have the same effect as brand-name drugs. Nurses also need to inform patients that generic drugs might look different (color, shape, or packaging), but the impact is the same.
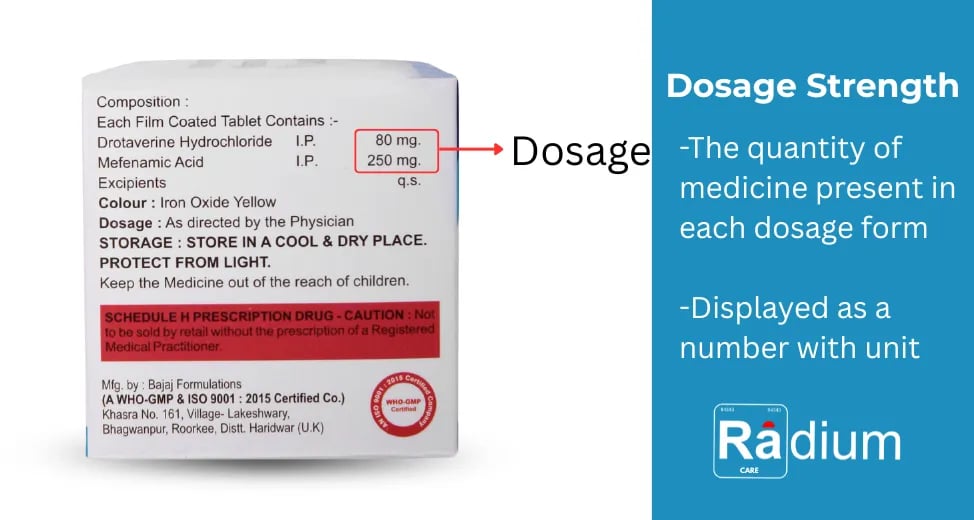
2. Dosage Strength
The strength of the dose on a packet of medicine informs you how much active medicine is contained in each unit, if this unit is a milliliter of liquid, a capsule, or a tablet.
Calmsol Tablet consists of:
Mefenamic Acid 250 mg
Drotaverine Hydrochloride 80 mg
What that means is that every single tablet holds these amounts of both active medicines.
Why it is important: Verifying the strength of the dosage is important because it guarantees that you use the drug in exactly the manner in which it was prescribed. If you take less than directed, it can decrease effectiveness and not treat the disease, yet taking more than recommended increases the possibility of inducing side effects or harm.
3. Route of Administration
The administration route on a medicine label informs you exactly how the medicine must come into your body. This is extremely important because each medicine works best when taken in one specific manner.
Some of the most frequent routes are:
Oral (by mouth): Pills, capsules, or liquids swallowed and absorbed by the stomach or intestines. This is the most frequent route.
Intravenous (IV, into a vein): Medicine given directly into the bloodstream for a rapid effect. Often used in hospitals.
Intramuscular (IM, into a muscle): Medicine administered into a big muscle (such as the arm or thigh), where it is slowly absorbed.
Subcutaneous (under the skin): A tiny injection just under the skin, e.g., insulin for diabetes.
Sublingual/Buccal (under the tongue or in the cheek): Drugs that disintegrate rapidly and get absorbed into the body via the bloodstream without passing through the stomach. Example: certain heart medications.
Topical (on skin): Ointments, creams, or gels put onto the skin for localized effect (such as rashes or pain).
Eye or Ear drops: Drugs placed in eyes for eye infections or ears for infection/pain.
Rectal or Vaginal Suppositories: Medication in solid state placed in the rectum or vagina and dissolves, being absorbed.
Inhalation (breathing): Inhalers or nebulizers give medication to the lungs themselves, which is useful in asthma and other conditions.
Transdermal (skin patches): A patch on the skin which releases medicine into the body for an extended period of time.
Why it matters: A pill that is supposed to be swallowed must not be injected, and one that is designed to be injected must not be swallowed. Getting it wrong can render the drug useless—or even harmful. For instance, injecting a tablet taken orally may clog up blood vessels, while swallowing an ointment or cream may lead to poisoning. Always do exactly as stated on the label.
4. Medication Forms
Medications are produced in diverse forms depending on treatment needs:
Tablets and capsules – most common solid dose form
Syrups or solutions – liquid form, often for children
Suspensions – liquid with particles that require shaking prior to use
Ointments, creams, gels – applied on skin surface
Injections – delivered directly into veins, muscles, or beneath the skin
Suppositories – administered rectally or vaginally for local or systemic effect
Release types:
Immediate release – work immediately after administration
Extended/controlled release – release medicine slowly over long time
Why it matters: Extended-release tablets should never be crushed or divided. This can release all the dose at once and cause a risk of overdose.
5. Lot Number & Expiration Date
Two label bits of information are essential to safety:
Lot Number: A number used to identify the batch of medicine. Used for tracking production and is essential in the event that a recall is made.
Expiration Date: The date the medicine will remain safe and effective until.
Why it matters: Expired medicines may lose effectiveness and/or become harmful. Be sure to check all of this prior to use.
6. Medication Instructions
Instructions for safe use are also given on labels, including:
How many times to take the medicine – once daily, twice a day, or as directed by the physician. Adherence to the timing is extremely crucial to have the correct amount of medicine in the body.
How to take it – before food, after food, or on an empty stomach. Some drugs are more effective when taken with food, while others can produce side effects if taken otherwise.
Storage conditions – store at room temperature, in a cool dry location, or refrigerate if stated. Storing drugs safely is critical to maintaining their potency until their expiration date.
Precautions and warnings – the labels might warn one not to consume the medicine with alcohol, drive after consumption, or use it with other medications. These warnings are put in place for the safety of the patient.
Why it is important: Medicines are designed and manufactured with specific conditions in mind. If they cannot meet their storage conditions, they cannot be guaranteed to work as intended.If the instructions are not followed, the medicine may not work as it should or, even worse, could cause harm.
7. Manufacturer & Distributor Information
The distributor/manufacturer name, always clearly stated on the label, ensures accountability and keeps healthcare providers or patients able to contact the right source should there be a quality issue.
At Radium Care, everything has transparent manufacturer information for transparency and trust.
8. Tips for Patients, Nurses, and Caregivers
For Patients: Always read the label first, ensure that the expired date has not expired, and never give medications to others. Discuss with your doctor or pharmacist if things are unclear.
For Nurses and Caregivers: Adhere to the “five rights” of medication administration:
Right patient.
Right drug.
Right dose.
Right route.
Right time.
Check all medications before you give the drugs to your patient, record all medications in the proper manner, and provide appropriate patient education for medications prescribed.
9. Prescription & Safety Warnings (Red Strip on Label)
Most drugs have a red warning strip on the label. It’s not a design element—it’s a medical and legal precaution.
For instance, Calmsol tablets indicate:
“SCHEDULE H PRESCRIPTION MEDICATION – WARNING: Not to be sold at retail except by or on the order of a Registered Medical Practitioner.”
What it means:
“Scheduling H” drugs are controlled under India’s Drugs and Cosmetics Act.
They are prescription drugs, and as such, you can’t obtain them over a counter.
These drugs need a doctor’s supervision to have a safe intake and avoid abuse.
Why it matters:
Avoids risks of self-medication (wrong treatment, wrong illness, side effects).
Saves patients from potential severe damage from unmonitored consumption.
Guarantees only trained medical professionals determine the appropriate treatment.
Takeaway: Respect the red strip warnings at all times. If your medication carries this warning, do not try to purchase or use it without seeking advice from a licensed physician.
Why Label Literacy Matters
Safe use of medicines is based on knowledge, accuracy, and responsibility. Whether you are a patient swallowing morning pills, a nurse giving an injection, or a family member giving medication in the home, the secret to safety is learning to read and understand a medicine label. It’s a quick habit that can prevent serious errors, reduce risks, and maintain overall well-being.
At Radium Care, we strongly believe that knowledge saves lives. By creating awareness on how to read and interpret medication labels, we want to ensure that each dose consumed is safe, effective, and actually beneficial for the recipient. Remember, the right medicine only works if it is consumed in the right manner, with the right strength, and at the right time.
Final Thoughts
Safe use of medication is based on awareness and precision. You may be a patient taking medication alone, a nurse administering an injection to you, or a caregiver administering tablets at home. No matter what you do, you will not make any mistakes and you will stay healthy as long as you can read and interpret a medication label. Our motto at Radium Care is that knowledge is life. By encouraging awareness about the drug label, we hope to make certain that every dose we consume is effective, safe, and worth it.
A drug label is not so much fine print — it’s a lifesaver. From brand name and dose strength to routes, instructions, and expiration dates, each piece of information counts. By knowing how to read labels appropriately, patients become empowered, and healthcare professionals provide safer care. Clear comprehension of labels also prevents taking the wrong dose, taking too much by accident, or taking outdated medicines. It makes sure that the drugs are kept well, handled well, and administered at the appropriate time.
At Radium Care, our purpose is to assist healthcare professionals and patients with credible products and verifiable information for a better tomorrow. We are of the opinion that safe healthcare starts with small, cautious steps — and reading the labels on medications is one of the most crucial of them.
And don’t forget: Never take or give medicine without the prescription and advice of a registered health practitioner.
Frequently asked questions
What can always be located on the label of a medicine?
A medicine label will always contain the brand name and generic name of the drug, dosage strength (amount of drug in each tablet/capsule), instructions for use (how many, how), route of administration (oral, injection, etc.), conditions for storage, expiry date, lot number, and safety warnings.
Why is knowing the dosage strength valuable?
Because it informs you exactly how much of the active ingredients are contained in each unit. That way, you can get the correct amount—not too small (which might not work) and not too large (which can be dangerous).
What is “route of administration”?
It is how the medicine gets into the body—by mouth, injection, skin patch, drops, etc. Taking the wrong route can make the medicine useless or even hazardous.
What do you do if an expiry date has already passed on a medicine?
Don’t use it at all. Expired medicines can weaken, or their chemical makeup may alter and may cause harm. Dispose of expired ones appropriately.
Phone no. +91-84343 84343
Support: [email protected]
Location: 40-GF, Harmony Mall, Goregaon (W), Mumbai – 400


A Gentle Touch for Motherhood
Pregnancy-safe, thoughtfully crafted skin and personal care solutions designed to support women through every stage of motherhood.
Quick Links
Get in Touch
